Table of Content
- G. Request for Information: Health Equity in the HH QRP
- Resumption of Care
- Table F1—U.S. Bureau of Labor Statistics' May 2020 National Occupational Employment and Wage Estimates
- Health Care Reform
- Table F2—CY 2020 OASIS Submissions by Time Point
- Listing Results about 2022 Home Health Lupa Rates
- Home Health Low Utilization Payment Adjustment (LUPA) Threshold Calculator
Beginning with the CY 2027 program year, HHAs will be required to report OASIS data on all patients, regardless of payer, for the applicable 12-month performance period . The final claim that the HHA submits for payment determines the total payment amount for the period and whether we make an applicable adjustment to the 30-day case-mix and wage-adjusted payment amount. The end date of the 30-day period, as reported on the claim, determines which calendar year rates Medicare will use to pay the claim. Several commenters stated cost inflation is at a 40-year high and HHAs report continuing labor cost increases in second quarter 2022 and third quarter 2022 that range from 7 to 12 percent. A commenter noted that a recent survey conducted by Dobson & Davanzo found higher labor cost growth than is reflected in the proposed market basket index, along with a significantly greater nurse labor cost increase as determined by the U.S. Department of Labor, Bureau of Labor Statistics average hourly earnings for home health industry, which showed year-over-year growth in the first quarter of 2022 of 5.2 percent.

No fee schedules, basic unit, relative values or related listings are included in CDT-4. The ADA does not directly or indirectly practice medicine or dispense dental services. The sole responsibility for the software, including any CDT-4 and other content contained therein, is with or the CMS; and no endorsement by the ADA is intended or implied.
G. Request for Information: Health Equity in the HH QRP
Based on our analysis, we conclude that the policies finalized in this rule would result in an estimated total impact of 3 to 5 percent or more on Medicare revenue for greater than 5 percent of HHAs. Therefore, the Secretary has determined that this HH PPS final rule will have significant economic impact on a substantial number of small entities. We estimate that the net impact of the policies in this rule is approximately $125 million in increased payments to HHAs in CY 2023. The $125 million in increased payments is reflected in the last column of the first row in Table F5 as a 0.7 percent increase in expenditures when comparing CY 2023 payments to estimated CY 2022 payments.
Section 1895 of the Act allows for the provision of an addition or adjustment to the home health payment amount otherwise made in the case of outliers because of unusual variations in the type or amount of medically necessary care. Under the HH PPS and the previous unit of payment (that is, 60-day episodes), outlier payments were made for 60-day episodes whose estimated costs exceed a threshold amount for each HHRG. The episode's estimated cost was established as the sum of the national wage-adjusted per visit payment amounts delivered during the episode. The outlier threshold for each case-mix group or PEP adjustment defined as the 60-day episode payment or PEP adjustment for that group plus a fixed-dollar loss amount. For the purposes of the HH PPS, the FDL amount is calculated by multiplying the home health FDL ratio by a case's wage-adjusted national, standardized 60-day episode payment rate, which yields an FDL dollar amount for the case.
Resumption of Care
The time period when the sun is no more than 6 degrees below the horizon at either sunrise or sunset. The horizon should be clearly defined and the brightest stars should be visible under good atmospheric conditions (i.e. no moonlight, or other lights). With our Flex rate, HRS customers can always cancel their hotel bookings free of charge before 6 pm on the check-in day. The hotel has undergone a self-inspection process on its enhanced protection measures.
Commenters believed that payment should not be tied to measure performance until a measure is thoroughly tested, evaluated, and has NQF-endorsement. They believe that measure methodology and implementation of individual measures should be sufficiently vetted prior to inclusion, and specifically part of the HH QRP prior to advancing to the expanded HHVBP Model. Commenters suggested that prior to adding new measures to value-based purchasing initiatives, measures should first be included in its related quality reporting program. After consideration of the public comments received, we are finalizing our proposals without modification. Measures; and the impact of the domains and quality measure concepts on organizational culture change.
Table F1—U.S. Bureau of Labor Statistics' May 2020 National Occupational Employment and Wage Estimates
Therefore, we proposed to reassign the ICD-10-CM diagnosis codes listed in Table 9 from clinical group E and clinical group A (MMTA-Other) to clinical group C . The following section proposed reassignment of 320 diagnosis codes to a different clinical group when listed as a principal diagnosis, reassignment of 37 diagnosis codes to a different comorbidity subgroup when listed as a secondary diagnosis, and the establishment of a new comorbidity subgroup for certain neurological conditions and disorders. Due to the amount of diagnosis codes proposed for reassignment this year, we posted the “CY 2023 Proposed Reassignment of ICD-10-CM Diagnosis Codes for HH PDGM Clinical Groups and Comorbidity Subgroups” supplemental file on the Home Health Prospective Payment System Regulations and Notices web page. The term itself stands for “Low Utilization Payment Adjustment,” which is a standard per-visit payment for episodes of care with a low number of visits.

In response to interested parties' questions regarding upper respiratory malignant neoplasms, we reviewed 14 ICD-10-CM diagnosis codes related to malignant neoplasms of the upper respiratory tract currently assigned to the comorbidity subgroup neoplasm 6 . We also determined that B78.9 strongyloidiasis, unspecified was assigned to clinical group C , and should be reassigned to clinical group K (MMTA—Infectious Disease, Neoplasms, and Blood-Forming Diseases) because it would be consistent with the assignment of the other strongyloidiasis codes. We also identified that N83.201 unspecified ovarian cyst, right side was assigned to clinical group A (MMTA—Other) and should be reassigned to clinical group J (MMTA—Gastrointestinal Tract and Genitourinary System) because it would be consistent with the assignment of other ovarian cyst codes. We proposed to reassign these two ICD-10-CM diagnosis codes' clinical groups as shown in Table 6.
For CY 2023 rate setting, we do not anticipate significant differences between using pre COVID-19 PHE data and the most recent claims data at the time of rulemaking . Therefore, we will continue our practice of using the most recent, complete utilization data at the time of rulemaking; that is, we are using CY 2021 claims data for CY 2023 payment rate updates. For CY 2023, we proposed to update the LUPA thresholds using CY 2021 Medicare home health claims linked to OASIS assessment data.
A professional mortgage specialist can help you set up your finances and provide a comprehensive breakdown of your maximum mortgage, required monthly payments, and closing costs. In addition, section 1102 of the Act requires us to prepare an RIA if a rule may have a significant impact on the operations of a substantial number of small rural hospitals. For purposes of section 1102 of the Act, we define a small rural hospital as a hospital that is located outside of a metropolitan statistical area and has fewer than 100 beds. Therefore, the Secretary has certified that this final rule would not have a significant economic impact on the operations of small rural hospitals. Commenters requested that CMS select measures that are reliable, reflect true differences in performance and are not attributable to random variation; and, consider outcome measures for the expanded Model related to beneficiary access and outcomes, as well as costs.
Our clinical advisors reviewed the three ICD-10-CM diagnosis codes related to lymphedema and determined that assessing and treating lymphedema is similar to the assessment and staging of wounds. It requires the assessment of pulses, evaluation of the color and amount of drainage, and measurement. In addition, some lymphedema can require compression bandaging, similar to wound care. Because of these similarities, we determined the reassignment of the three ICD-10-CM diagnosis codes related to lymphedema to clinical group C is clinically appropriate.
These standards could support the exchange and reuse of patient assessment data derived from the Minimum Data Set , Inpatient Rehabilitation Facility-Patient Assessment Instrument (IRF-PAI), LTCH Continuity Assessment Record and Evaluation Data Set , Outcome and Assessment Information Set , and other sources. The PACIO Project has focused on HL7 FHIR implementation guides for functional status, cognitive status and new use cases on advance directives, re-assessment timepoints, and Speech, Language, Swallowing, Cognitive communication and Hearing pathology. We encourage PAC provider and health IT vendor participation as the efforts advance. Under the Prospective Payment System , there was a single threshold — having to manage five visits over 60 days. Now, there are 432 thresholds to manage based on patient condition — and the time period is cut in half to just 30 days.
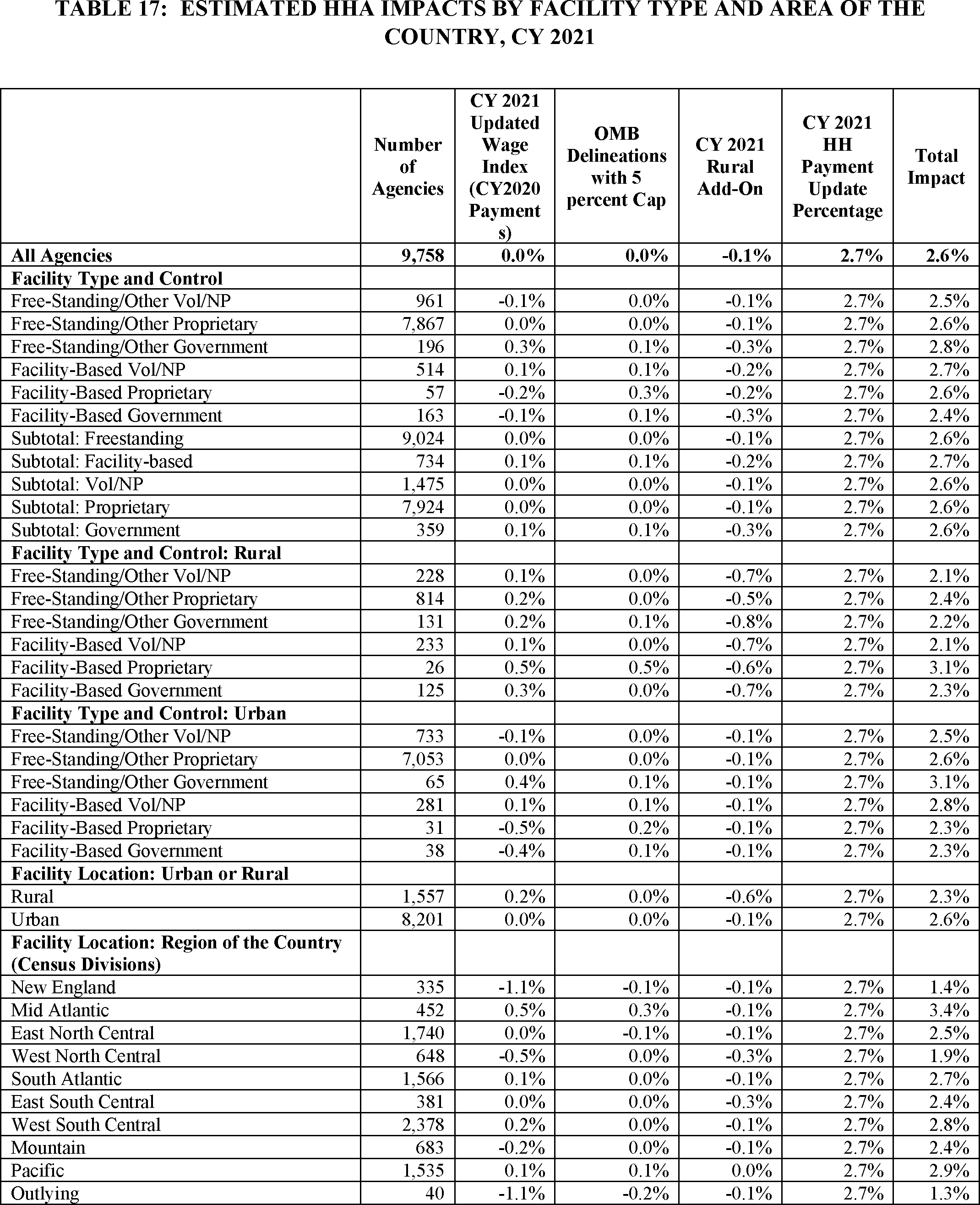
In the CY 2019 HH PPS final rule with comment period , we finalized our policy that the LUPA thresholds for each PDGM payment group would be reevaluated every year based on the most current utilization data available at the time of rulemaking. However, as CY 2020 was the first year of the new case-mix adjustment methodology, we stated in the CY 2021 HH PPS final rule that we would maintain the LUPA thresholds that were finalized and shown in Table 17 of the CY 2020 HH PPS final rule with comment period for CY 2021 payment purposes. We stated that at that time; we did not have sufficient CY 2020 data to reevaluate the LUPA thresholds for CY 2021.
The proposed recalibrated case-mix weights were updated based on more complete CY 2021 claims data for this final rule. With regard to therapy, CMS received comments in the CY 2022 HH PPS final rule and in response to the CY 2023 HH PPS proposed rule that the decrease in therapy utilization, including termination of therapy staff, is related to the removal of the therapy payment incentive. In their comment letter, a leading industry association detailed how HHAs have responded to changes in the benefit structure and have altered their operations, affecting the level of care received by patients. For instance, prior to the PDGM, the industry notes that HHAs were incentivized to provide the highest volume of therapy visits possible, and a low volume of other services. The industry association goes on to note that under the PDGM, the elimination of the therapy volume adjustment as a case mix measure will likely lead to a reduction in therapy services to patients. In an article published in February 2020, the National Association for Home Care and Hospice was quoted as saying “categorically, across the board, we're going to reduce our therapy services” as a result of the PDGM.
After reviewing the CY 2021 home health claims utilization data we determined that visit patterns have stabilized. We believe that CY 2021 data will be more indicative of visit patterns in CY 2023 rather than continuing to use the LUPA thresholds derived from the CY 2018 data pre-PDGM. Therefore, we proposed to update the LUPA thresholds for CY 2023 using data from CY 2021. We reviewed Q82.0 for clinical group reassignment, as described in section II.B.3.4. During this review, we discovered Q82.0 is not currently assigned to a comorbidity subgroup when listed as a secondary diagnosis.

No comments:
Post a Comment